Intracytoplasmic Sperm Injection (ICSI) is a form of assisted reproductive technology (ART) that has helped many couples overcome male infertility and achieve their dream of having a child. With advanced medical facilities and skilled professionals, Hyderabad has emerged as a preferred destination for ICSI treatment in India. If you and your partner are considering ICSI treatment in Hyderabad, it is important to understand what to expect throughout the process. This step-by-step guide will provide you with a comprehensive overview of ICSI treatment in Hyderabad, from the initial consultation to the embryo transfer, and help you prepare for this life-changing journey.
Initial Consultation: Understanding Medical History and Examining Reproductive Health
The initial consultation with a healthcare provider is a critical step in assessing an individual’s reproductive health. During this appointment, the healthcare provider will typically spend time understanding the individual’s medical history and conducting a physical examination to evaluate their reproductive health.
Understanding Medical History:
The healthcare provider will begin by asking the individual a series of questions about their medical history. This will include questions about their past and current medical conditions, medications, allergies, and surgeries. It is important to disclose all this information, as it can impact reproductive health and fertility. Additionally, the provider will ask about the individual’s menstrual history, including the age of onset, frequency, duration, and any symptoms such as pain or heavy bleeding. The healthcare provider may also ask about any sexual activity, contraceptive use, and any history of sexually transmitted infections (STIs).
Examining Reproductive Health:
After taking a thorough medical history, the healthcare provider will conduct a physical examination to evaluate the individual’s reproductive health. This typically includes a pelvic exam, which allows the healthcare provider to assess the health of the uterus, cervix, and ovaries. During the exam, the healthcare provider will use a speculum to open the vaginal walls and visualize the cervix. They may also collect samples for STI testing or a Pap smear to screen for cervical cancer. Additionally, the healthcare provider may conduct a breast exam to check for any abnormalities.
Depending on the individual’s medical history and exam findings, the healthcare provider may recommend further testing or refer the individual to a specialist for further evaluation and management. For example, if an individual has a history of irregular periods or infertility, the healthcare provider may recommend blood tests to check hormone levels or an ultrasound to evaluate the ovaries and uterus.
Overall, the initial consultation is an important step in understanding an individual’s reproductive health. It allows the healthcare provider to gather information about the individual’s medical history, perform a physical exam, and identify any potential issues that may impact reproductive health and fertility. By identifying any concerns early on, the healthcare provider can develop a personalized treatment plan and provide education on how to maintain optimal reproductive health.
Preparing for ICSI Treatment: Necessary Tests and Medications
Intracytoplasmic sperm injection (ICSI) is a specialized form of in vitro fertilization (IVF) that is used to treat infertility in couples. It involves the injection of a single sperm directly into the egg to fertilize it, which can be a successful treatment option for couples struggling with male factor infertility or other fertility issues. If you and your partner are considering ICSI treatment, here are some of the necessary tests and medications that you will need to prepare for:
- Fertility Testing: Before starting ICSI treatment, both partners will need to undergo a series of fertility tests to evaluate their reproductive health. These tests may include semen analysis for the male partner to check the quality and quantity of sperm, and blood tests for the female partner to evaluate hormone levels and egg quality. Additionally, a pelvic ultrasound may be done to evaluate the ovaries and uterus.
- Medications: Once the initial fertility testing is complete, the female partner will need to take medications to stimulate the ovaries and increase the number of eggs produced. These medications are typically given by injection and must be taken on a specific schedule. The healthcare provider will closely monitor the response to these medications through blood tests and ultrasounds to adjust the dosage if needed.
- Egg Retrieval: Once the follicles in the ovaries have reached an appropriate size, the female partner will undergo an egg retrieval procedure. This involves using a needle to remove the eggs from the ovaries under sedation. The eggs are then immediately taken to the laboratory for fertilization.
- Sperm Collection: On the day of the egg retrieval, the male partner will be asked to provide a semen sample. The sperm will then be washed and prepared for injection.
- ICSI Procedure: Once the eggs have been retrieved, they will be fertilized using the ICSI technique. A single sperm is injected directly into each egg using a tiny needle. The eggs are then closely monitored in the laboratory to determine if fertilization has occurred.
- Embryo Transfer: After 3-5 days of development in the laboratory, the embryos are transferred into the uterus using a thin catheter. The healthcare provider will closely monitor the patient for signs of pregnancy and may recommend additional medications or procedures to support implantation and development.
Ovarian Stimulation: Hormonal Therapy and Follicle Monitoring
Ovarian stimulation is an essential component of in vitro fertilization (IVF) and other assisted reproductive technologies. It involves using medications to stimulate the ovaries to produce multiple eggs, which can then be retrieved and fertilized in the laboratory. Here are the two key components of ovarian stimulation: hormonal therapy and follicle monitoring.
Hormonal Therapy:
Hormonal therapy is used to stimulate the ovaries to produce multiple mature eggs. The medication used is typically gonadotropins, which are injected subcutaneously (under the skin) over a period of 8-14 days. Gonadotropins contain follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which are naturally produced by the pituitary gland in the brain to stimulate the ovaries. The dosage and duration of hormonal therapy vary depending on the individual’s age, ovarian reserve, and response to treatment. It is important to closely monitor the response to hormonal therapy to prevent overstimulation of the ovaries, which can lead to complications such as ovarian hyperstimulation syndrome (OHSS).
Follicle Monitoring:
Follicle monitoring involves using ultrasound and blood tests to monitor the response of the ovaries to hormonal therapy. Ultrasound is used to visualize the ovaries and measure the size and number of follicles, which are fluid-filled sacs that contain the eggs. Blood tests are used to measure hormone levels, including estradiol (E2), which is produced by the growing follicles. Follicle monitoring is typically done every 2-3 days during ovarian stimulation to adjust the dosage of gonadotropins and prevent overstimulation. Once the follicles reach a certain size, a trigger shot of human chorionic gonadotropin (hCG) is given to stimulate the final maturation of the eggs and prepare them for retrieval.
Retrieval of Eggs: An Overview of the Procedure
Egg retrieval is a key step in vitro fertilization (IVF) and other assisted reproductive technologies. It involves the removal of mature eggs from the ovaries using a needle guided by ultrasound. Here is an overview of the egg retrieval procedure:
- Preparation: The patient will be given instructions on how to prepare for the procedure, including avoiding food and drink for a certain amount of time before the procedure. The patient will also receive anesthesia to help manage any discomfort during the procedure.
- Ultrasound: An ultrasound probe is used to visualize the ovaries and locate the mature follicles. The probe is inserted into the vagina and guided to the ovaries. The mature follicles will appear on the ultrasound as fluid-filled sacs.
- Needle Placement: Once the mature follicles are located, a thin needle is guided through the vaginal wall and into the follicle. The needle is attached to a suction device that will remove the fluid and the mature egg from the follicle. The process is repeated for each mature follicle.
- Egg Collection: The fluid and eggs are collected in a test tube and immediately taken to the laboratory for evaluation and preparation for fertilization.
- Recovery: After the procedure, the patient will be monitored for a short time before being discharged. It is recommended to have a companion to drive the patient home as the anesthesia may cause drowsiness.
- Follow-up: The healthcare provider will monitor the patient closely for any complications such as bleeding, infection, or ovarian hyperstimulation syndrome (OHSS). The patient may also receive instructions on how to care for themselves at home and when to return for the embryo transfer.
Collection and Preparation of Sperm: Techniques and Procedures
Collection and preparation of sperm are critical steps in vitro fertilization (IVF) and other assisted reproductive technologies. Here are the techniques and procedures involved in the collection and preparation of sperm:
1. Collection of Sperm: Sperm can be collected in various ways depending on the individual’s circumstances. The most common methods are:
- Masturbation: The man is asked to masturbate and ejaculate into a sterile container.
- Testicular Sperm Extraction (TESE): If the man has a low sperm count or a blockage in the reproductive tract, the sperm may be extracted directly from the testicles using a needle or biopsy.
- Epididymal Sperm Aspiration (PESA): This procedure is similar to TESE but involves extracting sperm from the epididymis, a small tube located next to the testicles.
- Electroejaculation: In some cases, men with spinal cord injuries or other neurological conditions may require electroejaculation, which involves using electrical stimulation to induce ejaculation.
2. Semen Analysis: Once the sperm is collected, it is analyzed to determine its quality, quantity, and motility. The analysis includes evaluating sperm count, volume, morphology (shape), and movement.
- Sperm Preparation: Sperm preparation is necessary to separate the healthy, motile sperm from the dead, immotile sperm and other debris. The most common techniques for sperm preparation include:
- Swim-up Technique: This technique involves adding the sperm to a special culture medium and allowing the motile sperm to swim up to the top.
3. Density Gradient Centrifugation: This technique involves layering the sperm over a gradient of different densities, which separates the motile sperm from the dead or immotile sperm.
4. Cryopreservation: In some cases, the sperm may be frozen and stored for future use. Cryopreservation involves adding a cryoprotectant solution to the sperm and slowly freezing it to -196°C. The sperm can be stored for several years and used for IVF or other assisted reproductive technologies.
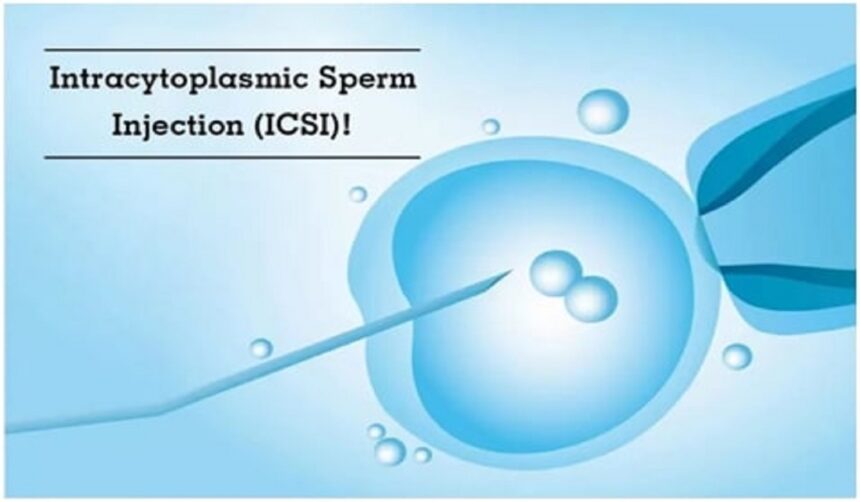
Intracytoplasmic Sperm Injection (ICSI): Fertilization of the Eggs
Intracytoplasmic Sperm Injection (ICSI) is a specialized technique used in assisted reproductive technology (ART) to fertilize eggs with a single sperm. Here’s an overview of the ICSI process:
- Egg Retrieval: Mature eggs are retrieved from the woman’s ovaries using a thin needle guided by ultrasound.
- Sperm Collection: A sperm sample is collected from the man through ejaculation, testicular sperm extraction (TESE), epididymal sperm aspiration (PESA), or electroejaculation.
- Sperm Preparation: The sperm sample is washed and prepared by removing the semen and other debris. Then, a single sperm is selected under a high-powered microscope.
- ICSI Procedure: The selected sperm is injected directly into the egg using a specialized pipette under a microscope. The egg is held in place by a holding pipette while the sperm is injected into the egg with a fine needle.
- Embryo Culture: The fertilized egg, now called an embryo, is cultured in a laboratory for several days to allow it to divide and grow.
- Embryo Transfer: Once the embryo has developed, it is transferred to the woman’s uterus, typically using a thin catheter guided by ultrasound.
ICSI is typically used when male factor infertility is present, such as low sperm count, poor sperm motility, or abnormal sperm morphology. It is also used in cases where conventional IVF has not been successful.
Embryo Culture: Growing and Monitoring the Embryos in the Lab
Embryo culture is an essential part of the in vitro fertilization (IVF) process, which involves growing and monitoring embryos in a laboratory until they are ready for transfer to the woman’s uterus. Here’s an overview of the embryo culture process:
- Fertilization: After the eggs have been retrieved and fertilized using either conventional IVF or intracytoplasmic sperm injection (ICSI), the resulting embryos are placed in a culture medium in a petri dish.
- Incubation: The petri dish is placed in a special incubator that provides a controlled environment with the right temperature, humidity, and pH levels.
- Embryo Development: The embryos are monitored daily by a trained embryologist to ensure that they are developing properly. The embryologist will evaluate the embryos based on factors such as the number of cells, their size and shape, and the appearance of the surrounding zona pellucida, a protective layer around the embryo.
- Embryo Grading: Embryos are graded based on their appearance and quality. This grading system helps the embryologist determine which embryos are most likely to result in a successful pregnancy.
- Embryo Selection: Depending on the number and quality of the embryos, the embryologist and the fertility specialist will decide which embryos to transfer to the woman’s uterus. In some cases, additional embryos may be frozen for future use.
- Embryo Transfer: Once the embryos have developed for several days and have been graded, the most viable embryo(s) are selected for transfer to the woman’s uterus. The transfer typically takes place three to five days after fertilization.
Embryo Transfer: Placing the Embryos into the Uterus
Embryo transfer is the final step in the in vitro fertilization (IVF) process and involves placing the embryos into the woman’s uterus. Here’s an overview of the embryo transfer process:
- Preparation: Before the embryo transfer, the woman may be given medications to prepare her uterus for implantation. This may include progesterone supplements or injections.
- Selection: The number and quality of embryos that are transferred depends on several factors, including the woman’s age, the number and quality of embryos available, and the preferences of the couple and the fertility specialist.
- Transfer: The transfer typically takes place three to five days after fertilization. The woman lies on her back with her feet in stirrups, and the fertility specialist inserts a thin, flexible catheter into the uterus through the cervix. The embryos are then placed into the uterus through the catheter.
- Post-Transfer: After the transfer, the woman may be asked to lie still for a short time to allow the embryos to settle. She may also be given additional medications, such as antibiotics, to help prevent infection.
- Follow-Up: The woman will typically return to the fertility clinic for a follow-up appointment to monitor her progress and check for signs of pregnancy. This may include blood tests to measure hormone levels and ultrasound scans to monitor the growth and development of the embryo(s).
Waiting for Results: The Two-Week Wait and Pregnancy Testing
After the embryo transfer, the woman enters a two-week waiting period before she can take a pregnancy test. This is known as the “two-week wait,” and it can be an emotional and stressful time for couples who are hoping to conceive. Here’s what you need to know about the two-week wait and pregnancy testing:
- Waiting Period: The two-week wait begins after the embryo transfer and lasts until the woman’s next menstrual period. During this time, she may experience symptoms such as mild cramping, bloating, and breast tenderness. However, it’s important to note that these symptoms can also be caused by the medications used during IVF and do not necessarily indicate pregnancy.
- Pregnancy Testing: After the two-week wait, the woman can take a pregnancy test to determine whether she is pregnant. Most clinics recommend waiting until the woman’s expected period date before taking a test to ensure accurate results. Home pregnancy tests work by detecting the presence of the hormone human chorionic gonadotropin (hCG), which is produced by the developing placenta after implantation.
- False Positives and Negatives: Home pregnancy tests are generally very accurate, but they can occasionally produce false-positive or false-negative results. A false positive occurs when the test indicates a positive result even though the woman is not pregnant. A false negative occurs when the test indicates a negative result even though the woman is pregnant.
- Blood Tests: If a home pregnancy test is positive, the woman will typically return to the fertility clinic for a blood test to confirm the pregnancy. Blood tests are more sensitive than home pregnancy tests and can detect lower levels of hCG. They can also be used to monitor the levels of hCG over time to ensure that the pregnancy is progressing normally.
- Coping with Negative Results: Unfortunately, not all IVF cycles result in a successful pregnancy. If the pregnancy test is negative, it’s important to seek emotional support and discuss the next steps with your fertility specialist. Some couples may choose to try another IVF cycle, while others may consider other options such as donor eggs or adoption.
Follow-Up Appointments and Next Steps: Monitoring Pregnancy and Addressing Any Concerns
After a successful embryo transfer and confirmation of pregnancy, the woman will need to attend follow-up appointments with her fertility specialist to monitor the pregnancy and address any concerns. Here’s what you can expect during these appointments:
- Ultrasound Monitoring: The first follow-up appointment typically takes place around six weeks after the embryo transfer. During this appointment, the woman will undergo an ultrasound to confirm the presence of a fetal heartbeat and to check the number of fetuses. Further ultrasounds will be scheduled throughout the pregnancy to monitor the growth and development of the fetus.
- Blood Tests: In addition to ultrasounds, the woman will also undergo regular blood tests to monitor hormone levels and ensure that the pregnancy is progressing normally.
- Managing Pregnancy Complications: Pregnancy after IVF is not without risk, and the woman may experience complications such as ectopic pregnancy, miscarriage, or preterm labor. If any complications arise, the fertility specialist will work closely with the woman’s obstetrician to manage the pregnancy and ensure the best possible outcome.
- Addressing Emotional Needs: Pregnancy after IVF can be an emotional rollercoaster, and it’s important to address any emotional needs or concerns that the woman may have. The fertility specialist may refer the woman to a therapist or support group to help her cope with the stress and uncertainty of pregnancy.
- Next Steps: Once the pregnancy is successfully completed, the fertility specialist will discuss the next steps with the couple, including options for future pregnancies and long-term follow-up care.
Conclusion
Shinefertility is a comprehensive fertility platform that provides information, resources, and support for couples who are struggling with infertility. The platform covers all aspects of fertility treatment, including initial consultations, ovarian stimulation, egg retrieval, sperm collection and preparation, ICSI, embryo culture, embryo transfer, and follow-up care. With Shinefertility, couples can access reliable information about fertility treatment and connect with experienced fertility specialists to guide them through each step of the process. The platform also offers emotional support and resources to help couples cope with the stress and uncertainty of infertility. Overall, Shinefertility is an excellent resource for couples who are seeking fertility treatment and looking to improve their chances of conceiving a healthy baby.