Embarking on the path to parenthood through fertility treatment like In Vitro Fertilization (IVF) is a significant step filled with hope and uncertainty. Gurgaon has become a major hub for fertility care in India, offering numerous clinics, advanced technologies, and experienced specialists.
This guide provides comprehensive, unbiased information to help navigate the landscape of IVF Centres in Gurgaon. It covers crucial aspects like clinic quality indicators, treatment costs, success rates, the patient journey, available technologies, and adherence to regulations like the Assisted Reproductive Technology (ART) Act, 2021, which ensures safety and ethical standards. The aim is to empower prospective parents with knowledge for informed decisions, without endorsing specific providers.
Top-Rated IVF Clinics in Gurgaon (2025)

While avoiding specific clinic names, understanding the hallmarks of high-quality IVF Centres in Gurgaon is vital. Excellence involves expertise, technology, patient support, and ethical practices.
Clinical Expertise and Experience
A reputable IVF centre relies on the experience of its entire clinical team – fertility specialists, embryologists, nurses, and counselors. Look for indicators like years of operation or the team’s collective experience. Successful IVF requires seamless coordination across disciplines.
The doctor’s diagnosis, the embryologist’s lab precision, the nursing team’s monitoring, and the counselor’s guidance are all interconnected. Assessing the entire multidisciplinary team’s quality is often more critical than focusing on one specialist’s reputation.
Advanced Technology and Laboratory Standards
The embryology lab is central to IVF success. State-of-the-art labs with advanced incubators, microscopes, and stringent air quality control are crucial for optimal embryo development. Some centres highlight internationally approved equipment or adherence to global standards. Significant investment in lab technology and quality control differentiates IVF Centres in Gurgaon.
Embryos are highly sensitive; a meticulously controlled lab environment minimizes risks like contamination and directly influences embryo viability. Clinics investing heavily in their labs are more likely to achieve better outcomes, like higher quality embryos and improved implantation rates. This focus on lab excellence is a critical quality benchmark.
Patient Care, Support, and Communication
The IVF journey is emotionally and physically demanding. High-quality clinics adopt a patient-centered approach, offering empathy and robust emotional support, often including psychological counseling. Clear, consistent communication is vital; the team should explain procedures, discuss risks/benefits, set realistic expectations, and be responsive.
Personalized treatment plans are also key. Practical aspects like clinic location, accessibility, and a comfortable environment contribute to the patient experience. Excellent patient care helps manage stress (which can affect outcomes) and ensures adherence to complex protocols, creating a more favorable environment for success.
Ethical Practices and Transparency
Ethical conduct and transparency are non-negotiable. This includes clarity on procedures, risks, realistic success rates, and comprehensive cost breakdowns. Adherence to national guidelines (ICMR, ART Act 2021) is mandatory. Be wary of clinics making unrealistic guarantees or being vague about costs.
True transparency involves proactively sharing all relevant information, enabling informed consent. This includes explaining test rationale, discussing individual success chances honestly, and providing access to medical records (scans, results, embryo photos). This openness builds trust and signifies ethical care. Patients should demand this clarity.
Accreditation and Compliance
Formal accreditations (e.g., NABH) or ICMR registration validate adherence to quality and safety standards. Some may hold international certifications (e.g., JCI). Compliance with the ART Act 2021 and Surrogacy (Regulation) Act 2021 is legally required, ensuring ethical operation.
Affordable IVF Treatment in Gurgaon (2025)
The financial aspect is a major consideration. Understanding the factors behind “IVF Cost in Gurgaon” and exploring “Affordable IVF Treatment Options in Gurgaon” is crucial.
Decoding the “IVF Cost in Gurgaon”
Costs vary dramatically, making an “average” price difficult. Estimates range from INR 25,000 – 68,000 for basic procedures to INR 1.4 Lakhs – 2.5 Lakhs for a standard cycle. Complex treatments (advanced tech, donor gametes, premium facilities) can push costs to INR 4-5 Lakhs or more per cycle.
This variation highlights the ambiguity of “IVF Cost.” Differentiate between basic self-cycles and complex scenarios involving ICSI, PGT, donor gametes, or multiple attempts, which are more expensive. Understanding the recommended treatment type is necessary for relevant cost estimates.
Key Cost Components
Total IVF Cost in Gurgaon includes several elements. Basic packages might cover initial consultations, some diagnostic tests (baseline ultrasounds, semen analysis), egg retrieval, standard lab fees (fertilization/culture), and embryo transfer.
Significant costs often excluded or variable include:
- Fertility Medications: Hormonal injection costs vary widely based on dosage/duration (influenced by age/ovarian reserve), forming a substantial expense.
- Diagnostic Tests: Comprehensive testing beyond basics (hormonal profiles, uterine evaluations, screening) may incur separate charges.
- Advanced Laboratory Techniques: ICSI, LAH, Blastocyst Culture, PGT, ERA usually carry additional fees.
- Gamete/Embryo Freezing and Storage: Cryopreservation (vitrification) involves initial freezing fees and ongoing annual storage charges. FET cycles have separate costs.
- Donor Services: Using donor eggs/sperm involves significant extra costs (recruitment, screening, compensation, procedures).
- Surgical Sperm Retrieval: PESA, TESA, TESE for male infertility add to the cost.
Factors Influencing Affordability
Clinic reputation/positioning (premium vs. budget), the specific treatment protocol (based on age, ovarian reserve, infertility cause), and the need for donor gametes or multiple cycles significantly impact the final IVF Cost in Gurgaon.
Finding Affordable Options & Financial Support
Many IVF Centres in Gurgaon promote “Affordable IVF Treatment Options in Gurgaon”. Scrutinize package inclusions carefully. To manage costs, clinics and financial institutions offer loans, financing plans, and EMI options, sometimes with 0% interest schemes. Exploring these can improve accessibility. Affordability considers more than one cycle’s cost, as success isn’t guaranteed initially. Budgeting might involve planning for multiple attempts.
Base costs often exclude significant expenses like high medication doses or advanced procedures. A low initial price might not reflect the final total. The availability of financing acknowledges this, helping manage potentially escalating costs. When seeking affordable care, consider the potential total outlay and investigate financial support.
Breakdown of IVF Cost in Gurgaon (2025)
| Component | General Price Range (INR) | Notes |
|---|---|---|
| Initial Consultation | ₹500 – ₹1,600+ | Per visit fee, may vary by specialist seniority |
| Diagnostic Tests (Pre-IVF) | ₹12,000 – ₹40,000+ | Includes Ovarian Reserve, Hormonal Profile, Scans, Semen Analysis etc. |
| Medications (per cycle) | ₹50,000 – ₹1,30,000+ | Highly variable based on patient response & protocol |
| Egg Retrieval Procedure | Included in cycle cost / Separate | May include OT, anesthesia, ward fees |
| Lab Fees (Fertilization/Culture) | Included in cycle cost / Separate | Covers standard IVF/ICSI lab work |
| Embryo Transfer Procedure | ₹40,000 – ₹1,50,000 / Included | Procedure cost, may include OT, embryologist fees |
| Embryo Freezing (Vitrification) | ₹14,000 – ₹90,000 (initial) | Plus annual storage fees (e.g., ~₹10,000) |
| Frozen Embryo Transfer (FET) | ₹40,000 – ₹1,50,000 per cycle | Cost for thawing and transferring frozen embryos |
| ICSI Add-on | ₹19,000 – ₹80,000+ | Additional cost over basic IVF |
| PGT (Preimplantation Genetic) | ₹40,000 – ₹1,70,000+ | Cost per batch of embryos tested |
| Laser Assisted Hatching (LAH) | ₹15,000 – ₹30,000 | Optional add-on procedure |
| Donor Egg Cycle | ₹2,50,000 – ₹4,50,000+ | Includes donor fees & associated procedures |
| Donor Sperm | ₹20,000 – ₹30,000+ add-on | Cost added to IVF/IUI cycle |
| Surgical Sperm Retrieval | ₹20,000 – ₹50,000+ | PESA/TESA/TESE procedures |
Note: These ranges are indicative based on available data and can vary significantly between clinics and individual cases. Always seek a detailed, personalized quote.
Best IVF Doctors in Gurgaon with High Success Rates
The fertility specialist is central, handling diagnosis, treatment strategy, key procedures (egg retrieval, embryo transfer), and cycle oversight. Understanding their qualifications and experience is key when evaluating IVF Centres in Gurgaon.

Common Qualifications
The pathway starts with an MBBS, followed by postgraduate OB-GYN (MD, MS, or DNB). Specialized training via a fellowship in Reproductive Medicine/Infertility (1-3 years) is crucial. Fellowships provide in-depth knowledge and practical skills in reproductive endocrinology, ART (IVF/ICSI), andrology, ultrasound, procedural experience (retrieval/transfer), and lab protocol observation.
Experience Matters
While qualifications are foundational, extensive practical experience is invaluable. Years of practice and cycles managed indicate proficiency. IVF involves intricate decision-making based on patient response. Seasoned specialists develop nuanced understanding to tailor protocols, troubleshoot challenges, and manage complex cases (poor ovarian response, recurrent failure, severe male infertility). Continuous learning and high case volume build expertise for optimizing outcomes, especially in difficult situations. Some specialists sub-specialize (e.g., genetics, male infertility).
Beyond Credentials: The Human Factor
Technical skill is paramount, but communication style, empathy, and patient-centeredness significantly impact the experience. A specialist who listens, explains clearly, and addresses concerns compassionately aids the stressful IVF journey, linking back to the clinic’s overall patient care quality.
Top IVF Success Rates in Gurgaon: Clinic Comparison & Key Factors
IVF success rates are key but require understanding what they represent and the influencing factors.
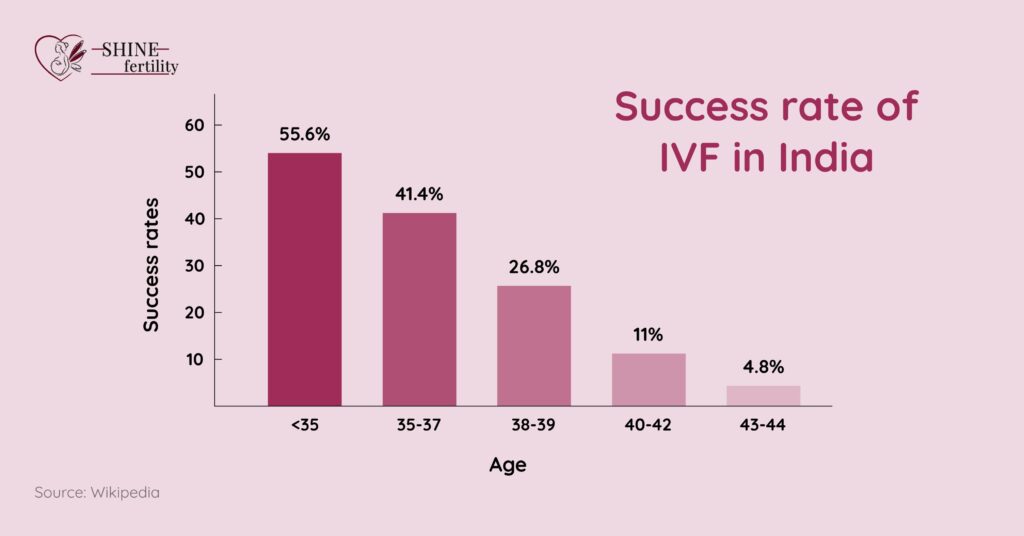
What Do Success Rates Mean?
Clinics report rates using different metrics: pregnancy rate (per cycle/transfer) or live birth rate (per cycle/transfer). The live birth rate (babies born per cycle) is most meaningful. Clinics may calculate data differently (specific patient groups, different denominators), making comparisons hard.
Seek clarification on calculation methods and applicable populations. General rates for IVF Centres in Gurgaon often range from 40% to over 70% per cycle, varying by clinic and patient factors, with some claiming rates exceeding national/international averages.
Factors Heavily Influencing Success
Numerous factors impact success:
- Age (Female): The most critical factor. Egg quantity/quality decline with age, affecting fertilization, development, and implantation.
- Cause of Infertility: Underlying reasons matter. Blocked tubes might have better IVF prognosis than poor egg quality.
- Reproductive History: Previous successful pregnancies are positive; recurrent miscarriages/failed IVFs suggest challenges.
- Lifestyle Factors: Smoking, excessive alcohol, obesity, or being underweight negatively impact fertility/IVF success. A healthy lifestyle is recommended.
- Embryo Quality: Developmental potential is crucial for implantation.
- Uterine Receptivity: The lining’s condition and ability to accept an embryo are vital.
- Sperm Quality: Male factors (count, motility, morphology) influence fertilization/development.
- Clinic Quality: Team expertise, lab standards, and technology contribute to success rates.
Setting Realistic Expectations
IVF doesn’t guarantee a baby. Success rates are probabilities. Many require multiple cycles. Clinics should discuss cumulative rates over several cycles. Be cautious of clinics promising 100% success or quoting high rates without context. While clinic-wide rates are benchmarks, individual chances depend heavily on personal factors (age, diagnosis).
Advanced tech like PGT can skew rates for specific groups (e.g., improving success per transfer for older patients). Donor eggs yield much higher rates (50-75%) for women with poor egg quality, largely independent of recipient age. Understanding how personal factors and treatment variations relate to overall statistics is essential for realistic expectations.
General IVF Live Birth Success Rate Ranges per Cycle (Own Eggs) in India/Gurgaon by Female Age
| Age Group | Typical Success Rate Range (%) | Key Considerations |
|---|---|---|
| < 35 | 40% – 60% | Highest potential due to better egg quality/quantity |
| 35 – 37 | 30% – 50% | Gradual decline in fertility begins |
| 38 – 40 | 20% – 40% | More significant decline in egg quality/quantity |
| 41 – 42 | 10% – 25% | Success rates decrease substantially |
| > 42 | < 15% | Significantly lower chances with own eggs |
Note: These ranges are approximate and based on general data reported in sources. Individual clinic rates and patient outcomes can vary. Donor egg cycles typically have higher success rates across older age groups.
What to Expect During IVF in Gurgaon: A Step-by-Step Patient Guide
IVF involves coordinated steps over several weeks. While protocols are tailored, the general pathway at most IVF Centres in Gurgaon is outlined below. A typical fresh cycle takes 3-6 weeks from medication start to pregnancy test.
Step 1: Initial Consultation and Evaluation
Begins with a detailed consultation (medical history, conception attempts, fertility issues). Diagnostic tests follow (blood tests for hormones/ovarian reserve, ultrasounds for ovaries/uterus, semen analysis, possibly uterine/tube tests). Evaluations determine infertility cause and guide the treatment plan.
Step 2: Ovarian Stimulation and Monitoring
Goal: produce multiple mature eggs. Achieved via fertility medications (daily injections +/- oral drugs). Response monitored closely via frequent blood tests (hormones) and ultrasounds (follicle number/size) over ~8-14 days. Dosages adjusted based on monitoring.
Step 3: Trigger Shot and Egg Retrieval
Once follicles are mature size, a “trigger shot” (hCG) induces final egg maturation. Egg retrieval scheduled ~34-36 hours later. Retrieval (follicular aspiration) is a minor surgery under sedation/anesthesia. Ultrasound guides a needle through the vaginal wall into ovaries to aspirate fluid/eggs.
Step 4: Sperm Collection and Preparation
Male partner provides fresh semen sample (or frozen donor sample thawed) on retrieval day. Lab processes sample to isolate healthy, motile sperm. Surgical retrieval (PESA/TESA) used if needed (e.g., azoospermia).
Step 5: Fertilization and Embryo Culture
Retrieved eggs combined with prepared sperm in the lab via conventional insemination or ICSI (single sperm injected into egg, common for male factor/previous failure). Fertilized eggs (embryos) cultured in incubators for 3-5 days. Many centres culture to blastocyst stage (day 5/6) for potentially higher implantation.
Step 6: Embryo Evaluation and Selection
Embryologists monitor development, assessing quality (cell division, appearance). If PGT planned, biopsy taken (usually blastocyst stage). Best-quality embryo(s) selected for transfer based on evaluation (+/- PGT results).
Step 7: Embryo Transfer
Selected embryo(s) placed into uterus. Simple, painless procedure (no sedation, mild cramping possible). Thin catheter passed through cervix into uterus under ultrasound guidance. Number transferred considered carefully (trend towards single embryo transfer – eSET – to minimize multiple pregnancy risks).
Step 8: Luteal Phase Support and Pregnancy Test
Woman takes medications (usually progesterone +/- estrogen) post-transfer to support uterine lining/implantation. Blood test (hCG) ~2 weeks later determines pregnancy.
Emotional and Physical Aspects
Physical discomforts (medication side effects like bloating, mood swings; minor post-procedure cramping) possible. Emotionally, it’s a rollercoaster (hope, anxiety, stress). Counseling and support systems are beneficial. The IVF journey is highly personalized; protocols and techniques are tailored based on monitoring and individual medical situation. This adaptability is key to optimizing success.
Best IVF Centres in Gurgaon with Advanced Fertility Technologies
Many IVF Centres in Gurgaon offer advanced technologies to address specific challenges and potentially enhance success for certain groups.
- Intracytoplasmic Sperm Injection (ICSI): Key for male factor infertility or previous fertilization failure. Single sperm injected directly into egg. IMSI (higher magnification sperm selection) also offered by some.
- Preimplantation Genetic Testing (PGT): Testing embryos before transfer. PGT-A (chromosomal abnormalities) aims to select normal embryos, potentially increasing implantation/transfer, reducing miscarriage/conditions like Down syndrome. PGT-M (specific inherited disorders) and PGT-SR (chromosomal rearrangements) also exist.
- Assisted Hatching (AH): Small opening made in embryo’s shell before transfer, potentially aiding implantation (sometimes for older patients, previous failures, frozen embryos). Lasers often used.
- Vitrification (Advanced Freezing): Flash-freezing for highly successful cryopreservation of eggs, sperm, embryos with excellent thaw survival. Enables fertility preservation and Frozen Embryo Transfer (FET) cycles, which can have high success rates.
- Blastocyst Culture: Culturing embryos to day 5/6 allows better selection of viable embryos, potentially improving implantation rates.
- Surgical Sperm Retrieval (SSR): For azoospermia, sperm retrieved directly from epididymis (PESA) or testes (TESA, TESE, Micro-TESE) for ICSI.
- Endometrial Receptivity Analysis (ERA): Uterine lining biopsy analyzes gene expression to determine personalized “window of implantation,” possibly for repeated implantation failures.
- Other Technologies: Time-Lapse Embryo Monitoring (e.g., EmbryoScope), Magnetic-Activated Cell Sorting (MACS) for sperm, Zona Birefringence microscopy may be used.
These technologies are tools, not universal solutions. Appropriate use depends on individual diagnosis/circumstances, based on evidence and specialist discussion. They often add complexity and cost. Patients should understand the rationale, potential benefits/drawbacks, and impact on total IVF Cost in Gurgaon.
Cost of IVF Treatment in Gurgaon: A Detailed Look
Key elements contributing to the final bill:
- Number of Cycles: Costs are per-cycle; multiple cycles multiply expense.
- Medication Dosage: Varies significantly; higher doses (often for age/low reserve) increase costs substantially.
- Use of Advanced Technologies: ICSI, PGT, ERA, AH etc., incur separate charges atop basic fees.
- Cryopreservation and FET: Freezing involves initial/annual fees; FET cycles charged separately.
- Donor Services: Using donor eggs/sperm adds considerable expense (recruitment, screening, compensation, procedures).
- Clinic’s Pricing Structure: Overheads, technology investment, pricing strategies influence package costs at different IVF Centres in Gurgaon.
The Crucial Role of Transparency
Transparency is paramount due to cost complexity/variability. Demand clear, detailed, itemized breakdowns before treatment. Be vigilant about “hidden costs”. Ask specific questions about package inclusions/exclusions (consultations, tests, meds, lab fees, freezing/storage, complications, follow-ups?). Clinics offering clear, fixed-price packages or transparent models provide predictability. This ethical approach builds trust.
Planning and Budgeting
Discuss financial concerns openly with clinic staff. Understand potential total cost (including contingencies for multiple cycles/advanced tech) for realistic budgeting. Explore financing/loans/EMI options early. Financial discussion needs personalization like medical consultation. Generic price lists are often insufficient.
Medication needs vary greatly. Transparent clinics should provide detailed quotes based on the specific proposed plan, including variations. Seeking itemized clarity helps avoid unexpected burdens and aids comparison of “Affordable IVF Treatment Options in Gurgaon”.
Conclusion
Navigating IVF Centres in Gurgaon requires careful consideration. Gurgaon is a major fertility hub offering a spectrum of options. Choosing the right centre involves more than success rates. Key factors include team expertise, lab quality/technology, patient care (communication, empathy, support), ethical practices, cost transparency, and regulatory compliance (ART Act).
Understanding the variable “IVF Cost in Gurgaon” necessitates seeking detailed breakdowns and exploring “Affordable IVF Treatment Options in Gurgaon” and financing. Interpreting success rates means considering individual factors (age, diagnosis) and the impact of advanced techniques/donor gametes. Familiarity with the IVF journey and technologies empowers decision-making. The IVF journey is personal.
Arming oneself with knowledge, asking questions, demanding transparency, and evaluating clinics based on quality markers helps individuals/couples make choices aligned with their needs, enhancing parenthood prospects. The path is complex, but informed choices and support offer hope.
Disclaimer:
The content provided in this blog regarding surrogacy and fertility treatments is intended solely for informational purposes and should not be interpreted as legal or medical guidance. Laws and regulations related to fertility and surrogacy can differ significantly by region and may evolve over time. We advise consulting with experienced legal and medical professionals to receive tailored advice suited to your individual circumstances. ShineFertility disclaims any liability for actions taken based on the information presented in this blog.



